
White matter lessions are associated with increases in blood pressure and global cognitive decline
 based on reviews by Isabel Garcia Garcia
based on reviews by Isabel Garcia Garcia
Progression of white matter hyperintensities is related to blood pressure increases and global cognitive decline – a registered report
Abstract
Recommendation: posted 22 April 2024, validated 22 April 2024
Chambers, C. (2024) White matter lessions are associated with increases in blood pressure and global cognitive decline. Peer Community in Registered Reports, 100717. https://doi.org/10.24072/pci.rr.100717
This is a stage 2 based on:
Frauke Beyer,Laurenz Lammer, Markus Loeffler, Steffi Riedel-Heller, Arno Villringer, Veronica Witte
https://osf.io/phctk
Recommendation
URL to the preregistered Stage 1 protocol: https://osf.io/qkbgj
List of eligible PCI RR-friendly journals:
The recommender in charge of the evaluation of the article and the reviewers declared that they have no conflict of interest (as defined in the code of conduct of PCI) with the authors or with the content of the article.
Evaluation round #1
DOI or URL of the report: https://osf.io/gmn6q
Version of the report: 1
Author's Reply, 12 Apr 2024
Dear Dr. García-García and dear Dr. Chambers,
thank you very much for your reviews and comments on the stage 2 manuscript.
Please find below my replies to your comments:
Comment 1: I highlighted the interpretation supported by the data in Table 7 in bold.
Comment 2: I was surprised by the lack of results regarding waist-to-hip ratio. In my experience, measuring waist-to-hip ratio can be prone to errors, specially in population datasets where multiple evaluators are involved. Have the authors checked if this variable correlates well with other indicators of obesity (such as visceral fat, if available in the dataset)? Was there any standardized operational procedure to ensure consistency across evaluators?
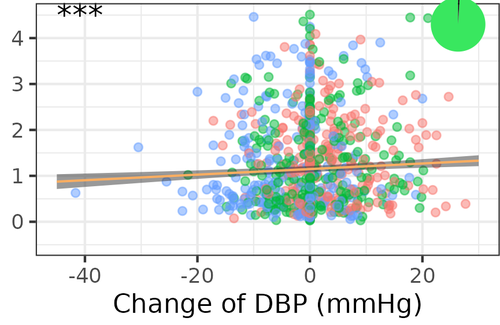
Answer: We agree that waist-to-hip ratio could be prone to errors where multiple raters might perfom the measurement differently. Standard operating procedures have been in place in the LIFE-Adult center to ensure that raters chose the same anatomical locations for waist and hip measurement, yet, there might be considerable variability. In a subset of 251 individuals from our cohort, we could check the association of WHR and visceral (VAT) and subcutaneous fat (SCAT) measured via abdominal MRI. There was a robust correlation of VAT and WHR (r=0.75), and a slightly smaller correlation of VAT divided by SCAT and WHR (r=0.62). We therefore believe that even though WHR might have been a slightly flawed measure, it still captured abdominal obesity fairly well in this sample. Also, higher WHR was related to higher WMH volume, although not nominally significant (e.g. Figure 2). A lack of power might therefore be the reason we did not detect a significant effect here. We edited the discussion accordingly.
Comment 3: When reporting the list of assessments related to executive functions, a description of semantic fluency is missing, while this variable appears right after in the calculation of the index.
Answer: We added a sentence describing the tests used from the CERAD battery, including the Animals-Test for semantic fluency.
Comment 4: The authors were clear and transparent regarding how missing data has been handled and inputed. Perhaps in Table 1 they could include the percentage of data that was missing for each variable.
Answer: We agree that this has not been clearly reported, and also realized that numbers of imputed data points depended on baseline and followup assessments. We therefore expanded Table 1 to include the number of available datapoints (N) per measure and timepoint. CESD was the variable with highest amount of missing, and antihypertensive medication had more missings at followup than baseline.
Looking forward to your response and with best wishes,
Frauke Beyer
Decision by Chris Chambers , posted 18 Mar 2024, validated 18 Mar 2024
, posted 18 Mar 2024, validated 18 Mar 2024
One of the reviewers from Stage 1 was available to assess your completed Stage 2 submission, and I have decided based on this evaluation and my own reading that we can proceed with an interim Stage 2 decision. As you will see from the enclosed comments, the reviewer is broadly satisified with your submission -- I concur and feel that it is already very close to meeting the Stage 2 criteria. The reviewer offers some useful remarks for consideration in a revision/response.
In addition to addressing these points, I would also recommend adding a column to the right of the study design table (Table 7) that reports the outcome in each case (i.e. whether the hypothesis was confirmed or disconfirmed).
I look forward to receiving your revised submission and response.
Reviewed by Isabel Garcia Garcia , 14 Mar 2024
, 14 Mar 2024
This longitudinal study examines the associations between blood pressure, abdominal obesity, and progression of white matter hyperintensities progression after 6 years in a community-dwelling population with a mean age of 63 years, and with a relatively low burden of white matter hyperintensities at baseline (1.88 cm3). The power analyses was extensively described, and I appreciated that the authors presented results from both linear models using change scores and linerar mixed models, and discussed the small differences of results obtained with each analysis.
Overall, this is an excellent study and I only have a few minor comments:
- I was surprised by the lack of results regarding waist-to-hip ratio. In my experience, measuring waist-to-hip ratio can be prone to errors, specially in population datasets where multiple evaluators are involved. Have the authors checked if this variable correlates well with other indicators of obesity (such as visceral fat, if available in the dataset)? Was there any standardized operational procedure to ensure consistency across evaluators?
- When reporting the list of assessments related to executive functions, a description of semantic fluency is missing, while this variable appears right after in the calculation of the index.
- The authors were clear and transparent regarding how missing data has been handled and inputed. Perhaps in Table 1 they could include the percentage of data that was missing for each variable.
https://doi.org/10.24072/pci.rr.100717.rev11










